Ultrasound therapy: more versatile than you think
From tendons to mastitis: ultrasound therapy’s evolving role in care.

We live in a time of rapid innovation and technological progress. However, that doesn’t mean classic (and trusted) techniques like ultrasound therapy are disappearing. On the contrary, the value of ultrasound reaches so much further than many people think. To rediscover this true and tried classic, we discuss below one widely recognized and two little-known (and perhaps even surprising ) applications of ultrasound therapy.
Quick refresher: what exactly is ultrasound therapy?
Ultrasound therapy is a safe treatment technique that uses sound waves to achieve therapeutic effects such as pain reduction, muscle relaxation, and tissue repair. It’s a non‑invasive and painless technique that’s drug‑free, easy to apply and has no proven adverse effects. With its tried and tested effectiveness, there is no reasons to leave ultrasound therapy out of your treatment toolkit.
Find out more about ultrasound therapy
The best‑known application of ultrasound: tendon disorders
The very first thing that comes to mind when you think of ultrasound therapy and are not quite familiar with what it is and can do, is probably the aspect of tendon problems. As a matter of fact, tendon disorders are indeed best‑known for the application of ultrasound therapy. To be more precise, low‑intensity ultrasound (LIUS) supports tendon healing, improves tensile strength, promotes better alignment of tendon fibres and increases cell proliferation [1]. That’s exactly why clinicians often use ultrasound therapy to improve pain levels, range of motion (ROM) and function in patients with, for example, subacromial impingement [2] or even Achilles tendinopathy plantar fasciitis [3] . But the many possibilities of applying ultrasound extend much further than that. Other disorders such as myofascial pain syndrome and even mastitis are aptly suited for the application of ultrasound therapy.

Ultrasound therapy for myofascial pain syndrome
Myofascial pain syndrome (MPS) can arise from excessive tension or a muscle injury and causes chronic muscle pain with a fixed referral pattern due to the formation of myofascial trigger points—a complaint that many patients visiting physiotherapist practices present with today.
Fortunately, ultrasound therapy has a demonstrated effect in MPS. In 2024,[4] Li et al. conducted a systematic review of RCTs examining the application of ultrasound therapy for MPS. They concluded that LIUS effectively reduces pain and improves the range of motion in patients suffering from MPS. Importantly, treatment parameters such as frequency, intensity and duration were heterogeneous throughout the examined studies, but most of them used a treatment frequency of approximately 1 MHz, increased the intensity to 1.5 W and chose a treatment time of 5 minutes. According to the authors, these values can be used to treat MPS effectively until there is more consensus on precisely which parameters to choose when treating MPS.
That sounds like the ideal package—but do patients experience it that way too? Mirjam certainly does:
“I regularly visit my physiotherapist for pain caused by trigger points. Other treatment techniques are too painful for me during an acute episode, and that pain hinders me in performing my exercises. After ultrasound therapy, however, the pain is sufficiently reduced so that my physiotherapist can switch to other techniques again and I can do my exercises better at home.”
Ultrasound for mastitis
Ultrasound therapy for mastitis may be the least known application, but it is no less promising. Mastitis is an inflammation of the mammary glands that affects 2–20 % of breastfeeding women every year. This painful [5] inflammation, which is often accompanied by fever, is usually treated with antibiotics. However, many physiotherapists are unaware that ultrasound therapy can also make a significant difference in mastitis and may sometimes even render antibiotics completely unnecessary.
Although there is (as of yet) little scientific evidence for the effectiveness of ultrasound therapy for treating mastitis, it is already being used in many physiotherapy practices worldwide. And when you think about it, that makes perfect sense: it is a therapy modality that’s easy to apply, painless and—as part of a physiotherapy regime—very accessible.
A retrospective pilot study in the Netherlands[6]
Between 2011 and 2014, Christiane Vreede‑van Iersel treated 17 mothers with mastitis by using ultrasound therapy. The treatment Christiane used, involved moving the applicator in circular motions from the outer edge of the induration towards the centre. The patient should feel no pain or tingling sensation.
Christiane used the following treatment parameters:
-
Treatment intensity : 1.0–2.5 W/cm²
-
Treatment frequency: 1 MHz
-
Applicator head surface: 5 cm²
-
Pulsed mode, duty cycle: 1:1
-
Treatment duration*: 1 minute per ultrasound head area
-
Treatment frequency: repeated on a daily basis

Christiane continued the treatments until the fever had resolved, the VAS had decreased with more than 3 points and was below 3, and swelling had been reduced by at least 50%. In her patients, this result was achieved after an average of six treatments.
We asked Christiane about her experience:
“Because of the beneficial effect of ultrasound therapy, you end up with a lot of happy mothers. Furthermore, there are no downsides for the patient. However, for the therapist, there is one small caveat that one has to take into account: the acute nature of mastitis requires flexibility—both in scheduling and in treatment location.”

Mobility and flexibility thanks to the Ultrasound compact
It’s a great feeling to be able to help new mothers so effectively. Unfortunately, many ultrasound devices are not suitable for home visits. But Gymna’s user‑friendly Ultrasound compact is. Because it’s able to operate on both battery and mains power, the Ultrasound compact can be used both inside and outside the clinic. Thanks to its small size (21×16×9 cm), its light weight of less than one and a half kilos, the Ultrasound compact is very easy to carry, wherever you go. The Gymna Ultrasound compact truly lives up to its name.
Ensuring safety and effectiveness with DynamUS
If you opt for ultrasound therapy to help your patients, you want to do so safely and effectively. That’s why all Gymna treatment heads are equipped with DynamUS, a motion‑detection system that helps you maintain the correct dynamic movement speed. With this nifty feature, the orange LED on the treatment head will warn you if your pace is too high or too low. At too high a pace, your treatment risks being ineffective; at too low a pace, your patient may be at risk of hotspots and internal tissue damage. That’s where the DynamUS feature comes in handy and helps you avoid these issues.
Save time thanks to your ultrasound device
As a physiotherapist, you undoubtedly always have plenty to do, so every time‑saving feature and nifty trick helps. With the Ultrasound compact, time savings come from both expected and unexpected angles:
-
User‑friendly interface: intuitive operation for everyday use
-
Wide viewing angle: the touchscreen is easy to read wherever you stand
-
High‑quality 7‑inch capacitive touchscreen: the flat surface is easy to clean and even disinfect
-
Magnetic, non-slip applicator holder: quickly and safely store your treatment heads
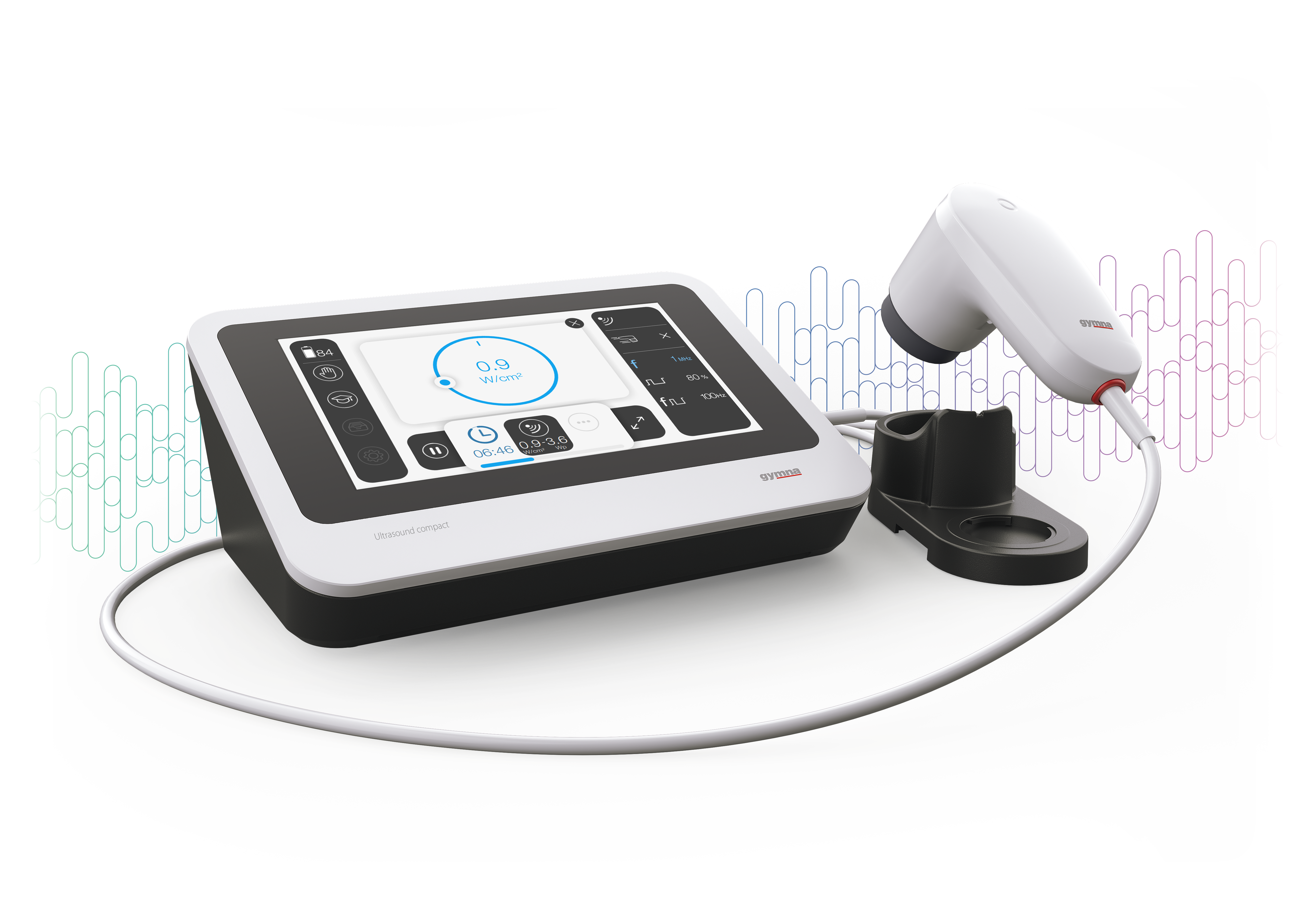
Did you know you can connect two treatment heads to the Gymna Ultrasound compact at the same time? This lets you switch between ultrasound heads easily, which not only saves time but also reduces cable wear. That’s two quick wins!
View the Gymna Ultrasound compact
Would you like to offer (mobile) ultrasound to your patients too?
Classic ultrasound therapy is still very relevant today—and (as you’ve read above) more versatile than you might come to expect. Would you like to add ultrasound to your treatment arsenal, or are you interested in upgrading your current ultrasound device to a mobile, compact model to make your work just that little bit easier? Feel free to contact us. We’ll be happy to advise you on expanding and improving your capabilities.
* The treatment duration was determined by the size of the induration. For each ultrasound‑head area, 1 minute of full ultrasound was applied, taking the duty cycle into account. Thus, for a treatment area of 10 cm², with a 5 cm² head and a duty cycle of 1:1, the treatment duration was 10/5 × 60 × 2 = 240 s = 4 minutes.
[1] Best, T. M., Wilk, K. E., Moorman, C. T., & Draper, D. O. (2016). Low Intensity Ultrasound for Promoting Soft Tissue Healing: A Systematic Review of the Literature and Medical Technology. Internal medicine review (Washington, D.C. : Online), 2(11), 271. https://doi.org/10.18103/imr.v2i11.271
[2] Calis, H. T., Berberoglu, N., & Calis, M. (2011). Are ultrasound, laser and exercise superior to each other in the treatment of subacromial impingement syndrome? A randomized clinical trial. European journal of physical and rehabilitation medicine, 47(3), 375–380.
[3] Alhakami, A. M., Babkair, R. A., Sahely, A., & Nuhmani, S. (2024). Effectiveness of therapeutic ultrasound on reducing pain intensity and functional disability in patients with plantar fasciitis: a systematic review of randomised controlled trials. PeerJ, 12, e17147. https://doi.org/10.7717/peerj.17147
[4] Li, X., Lin, Y., He, P., & Wang, Q. (2024). Efficacy and safety of low-intensity ultrasound therapy for myofascial pain syndrome: a systematic review and meta-analysis. BMC musculoskeletal disorders, 25(1), 1059. https://doi.org/10.1186/s12891-024-08174-7
[5] Wilson, E., Woodd, S. L., & Benova, L. (2020). Incidence of and Risk Factors for Lactational Mastitis: A Systematic Review. Journal of human lactation: official journal of International Lactation Consultant Association, 36(4), 673–686. https://doi.org/10.1177/0890334420907898
[6] Vreede van Iersel, C. (2015). Behandeling van mastitis met ultrageluidtherapie: een retrospectieve pilotstudie. Fysiopraxis, 24(1), 28-29.
